01. Delving into Inflammation and the Immune System
Introduction and Overview
Inflammation is a fundamental response by the body's immune system to protect against harm, such as infections, injuries, and toxins, initiating the process of healing. While typically beneficial in acute situations, when inflammation becomes chronic, it can lead to severe health consequences, contributing to a range of diseases, including heart disease, diabetes, and cancer. Understanding the dual nature of inflammation—its roles in both protecting and potentially harming the body—is crucial for managing health and preventing disease.
Inflammation Explained
Inflammation is the immune system's response to harmful stimuli, characterized by redness, heat, swelling, pain, and loss of function. This process is essential for the body's healing and defense mechanisms, involving a complex network of signaling molecules and cells that work to eliminate the cause of cell injury, clear out dead cells, and initiate tissue repair. However, when inflammation persists beyond the initial response to injury or infection, it can become chronic and contribute to the progression of various diseases.
A deeper understanding of inflammation's role in wound repair has emerged, indicating both beneficial and detrimental effects. Research has elucidated the molecular and cellular mechanisms controlling inflammation in cutaneous tissue repair, emphasizing the importance of targeting the inflammatory phase to modulate the healing outcome. For instance, Eming, Krieg, and Davidson (2007) highlighted the pivotal role of inflammation in establishing cutaneous homeostasis following injury, but also the potential for inflammation to delay healing and increase scarring, pointing to the complexity of inflammation's impact on tissue repair (Eming, Krieg, & Davidson, 2007).
Your Immune System Explained
The immune system is a sophisticated defense mechanism that protects the body against external threats, such as bacteria, viruses, and toxins, as well as internal threats, like cancer cells. It comprises two main components: the innate immune system, which provides immediate but non-specific defense, and the adaptive immune system, which provides a targeted response to specific pathogens. The innate system is the first line of defense and is responsible for the initial inflammatory response. In contrast, the adaptive system involves the creation of memory cells that recognize and respond more efficiently to previously encountered pathogens.
The inflammatory process is integral to the immune system's function, facilitating the removal of harmful stimuli and initiating tissue repair. Key players in the inflammation process include white blood cells (leukocytes), such as macrophages and neutrophils, which engulf and destroy pathogens. Cytokines, signaling proteins released by cells, play crucial roles in mediating and regulating the inflammatory response.
In the context of wound healing, inflammation is the first step, followed by tissue formation and remodeling. The immune system's regulation of inflammation is complex, with a balance between pro-inflammatory and anti-inflammatory signals ensuring proper healing. Excessive or prolonged inflammation can disrupt this balance, leading to impaired wound healing and chronic inflammation, underscoring the importance of understanding and potentially modulating the immune response to promote health and prevent disease.
The intricate relationship between inflammation and the immune system is central to the body's ability to heal and defend itself. Research continues to unravel the complexities of this relationship, aiming to harness the beneficial aspects of inflammation for healing while mitigating its harmful effects.
In the next chapters, we will explore how inflammation transitions from a protective mechanism to a potential pathogenic factor in various diseases, and the implications for treatment and prevention strategies.
02. When Good Inflammation Goes Bad
Introduction
While inflammation is a protective and healing response by the body to injury or infection, it can become harmful when it persists beyond its useful phase. Chronic inflammation is at the heart of many diseases that afflict people, from cardiovascular diseases to cancer and beyond. This shift from a beneficial to a detrimental state underscores the complex role of inflammation in health and disease.
Problem Inflammation
Chronic inflammation is a silent but potent factor in the development of various diseases. It acts through different mechanisms, including the persistent activation of inflammatory pathways, the production of inflammatory molecules, and the recruitment of immune cells that, instead of resolving the inflammation, contribute to tissue damage and dysfunction. This persistent state of inflammation can lead to DNA damage, promote cell proliferation, inhibit apoptosis (programmed cell death), and encourage angiogenesis (formation of new blood vessels), all of which can set the stage for cancer and other chronic diseases.
One notable example is the link between chronic inflammation and cardiovascular, metabolic, and renal diseases. Manabe (2011) highlights how obesity-induced chronic local inflammation in adipose tissue plays a crucial role in the development of heart failure and chronic kidney disease, underscoring the interconnectedness of chronic diseases through inflammatory processes (Manabe, 2011).
Further, Furman et al. (2019) discuss how social, environmental, and lifestyle factors can promote systemic chronic inflammation (SCI), leading to diseases that collectively represent the leading causes of disability and mortality worldwide, such as cardiovascular disease, cancer, diabetes mellitus, chronic kidney disease, non-alcoholic fatty liver disease, and autoimmune and neurodegenerative disorders (Furman et al., 2019).
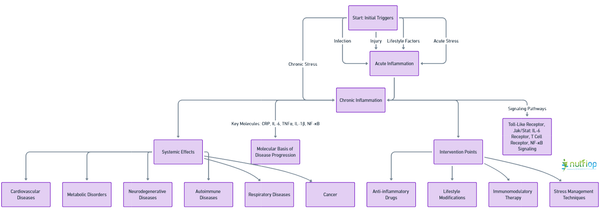
Interactive Disease Chart
This interactive disease chart illustrates the pathways through which chronic inflammation contributes to a wide range of diseases. It shows how initial triggers such as infection, injury, or lifestyle factors can evolve into a chronic inflammatory state, outlining the downstream effects on different body systems and highlighting potential intervention points to prevent disease progression.
Section 2 Quiz
1. True or False: Acute inflammation always leads to chronic inflammation.
2. Which of the following diseases is not typically associated with chronic inflammation?
a. Type 2 diabetes
b. Alzheimer's disease
c. Acute appendicitis
d. Cancer
3. What role does obesity play in chronic inflammation?
a. It has no effect on inflammation.
b. It reduces chronic inflammation.
c. It induces chronic local inflammation in adipose tissue.
d. It immediately resolves inflammation.
4. Which of the following factors does not promote systemic chronic inflammation (SCI)?
a. Physical injury
b. Poor diet
c. Regular exercise
d. Psychological stress
Click here to reveal the answers.
Answers: 1. False, 2. c, 3. c, 4. c
Understanding the transition from beneficial acute inflammation to harmful chronic inflammation provides critical insights into disease mechanisms and offers potential strategies for early diagnosis, prevention, and treatment. By addressing the underlying causes and processes of chronic inflammation, it may be possible to mitigate its contribution to a wide array of chronic diseases.
03. Inflammation and Allergic Responses
Introduction
Allergic inflammation is a complex immune response triggered by exposure to allergens. Unlike the beneficial inflammation that aids in healing, allergic inflammation is an overreaction of the immune system to harmless substances like pollen, dust mites, or certain foods. This overreaction can lead to a variety of allergic diseases, including hay fever, eczema, and asthma, affecting a significant portion of the population worldwide.
Allergies and Inflammation
The process of allergic inflammation involves the activation of various immune cells such as mast cells, eosinophils, and T lymphocytes. Upon exposure to an allergen, individuals with sensitivities produce Immunoglobulin E (IgE) antibodies that bind to receptors on mast cells and basophils. This binding triggers the release of histamine and other inflammatory mediators, leading to symptoms such as swelling, redness, and itching. The role of IgE and mast cells in initiating allergic responses underscores the intricate relationship between the immune system and allergens (Barnes, 2011).
Eczema and Asthma
Eczema (atopic dermatitis) and asthma are chronic conditions characterized by allergic inflammation. Eczema manifests as itchy, inflamed skin, while asthma affects the airways, leading to breathing difficulties. Both conditions are driven by type 2 immune responses, involving Th2 cells and cytokines like IL-4 and IL-13, which promote IgE production and eosinophil activation. The cross-talk between innate and adaptive immune responses, involving cells such as mast cells, basophils, and group 2 innate lymphoid cells (ILC2s), plays a crucial role in the pathology of these diseases (Kubo, 2017).
Treatment
The management of allergic inflammation primarily involves avoiding known allergens and using medications to control symptoms. Corticosteroids are effective in reducing inflammation, while antihistamines can alleviate itching and swelling by blocking histamine action. For chronic conditions like asthma and severe allergies, immunotherapy may be employed to gradually desensitize the immune system to specific allergens.
Section 3 Quiz
1. Which immune cells play a key role at the onset of an allergic response?
A) B lymphocytes
B) Mast cells and eosinophils
C) Red blood cells
D) Platelets
Click here to reveal the answer.
Correct Answer:: B) Mast cells and eosinophils
Explanation:
Mast cells and eosinophils are crucial in the initial stages of an allergic response. Upon exposure to an allergen, these cells are activated and release inflammatory mediators like histamine, leading to typical allergic symptoms.
2. What is the function of Th2 cytokines in the context of allergic diseases such as eczema and asthma?
A) They decrease the production of IgE.
B) They facilitate the activation of Th1 cells.
C) They promote IgE production and eosinophil activation.
D) They suppress mast cell degranulation.
Click here to reveal the answer.
Correct Answer:: C) They promote IgE production and eosinophil activation.
Explanation:
Th2 cytokines, including IL-4 and IL-13, are pivotal in driving type 2 immune responses characteristic of allergic conditions by promoting IgE production and eosinophil activation. This exacerbates the allergic inflammation seen in eczema and asthma.
3. Describe the role of Immunoglobulin E (IgE) in allergic inflammation.
A) It binds to antigens to prevent allergic reactions.
B) It is produced as a response to non-allergic stimuli.
C) It binds to receptors on mast cells and basophils, triggering the release of inflammatory mediators.
D) It deactivates eosinophils and reduces inflammation.
Click here to reveal the answer.
Correct Answer:: C) It binds to receptors on mast cells and basophils, triggering the release of inflammatory mediators.
Explanation:
IgE plays a central role in allergic reactions. Individuals with allergies produce IgE antibodies that bind to receptors on mast cells and basophils. This interaction causes the cells to release various inflammatory mediators, leading to allergic symptoms.
4. What are effective treatment strategies for managing allergic inflammation?
A) Increasing exposure to allergens
B) Use of corticosteroids and antihistamines
C) Administration of antibiotics
D) Avoidance of anti-inflammatory medications
Click here to reveal the answer.
Correct Answer:: B) Use of corticosteroids and antihistamines.
Explanation:
Managing allergic inflammation often involves avoiding known allergens and employing medications to control symptoms. Corticosteroids reduce inflammation, while antihistamines alleviate itching and swelling by blocking the action of histamine. For chronic or severe allergies, immunotherapy may also be considered to gradually desensitize the immune system to specific allergens.
Understanding the mechanisms of allergic inflammation is essential for developing targeted therapies to treat and prevent allergic diseases effectively. Research continues to unravel the complex interactions between immune cells, mediators, and environmental factors in allergic responses, offering hope for new and improved treatments.
04. Inflammation and Autoimmune Disease
Introduction
Autoimmune diseases arise when the immune system mistakenly targets the body's own cells, leading to chronic inflammation and various health issues. These conditions can affect almost any part of the body, including joints, skin, brain, and internal organs, resulting in a wide range of symptoms and complications.
When Your Body Fights Itself
The pathogenesis of autoimmune diseases involves a complex interplay between genetic predispositions and environmental triggers, leading to a breakdown in immunological tolerance. Central to this process is the role of inflammation, which not only serves as a response to tissue injury but, in the context of autoimmune diseases, contributes to tissue damage. For instance, a gain-of-function mutation in phospholipase C gamma 2 can cause severe spontaneous inflammation and autoimmunity by increasing external Ca2+ entry, highlighting the genetic basis of such diseases (Yu et al., 2023). Similarly, dysregulated Toll-like receptor (TLR) pathways, which are crucial for innate immunity, have been implicated in various autoimmune diseases, underscoring the role of innate immune responses in the development of autoimmunity (Chen, Szodoray, & Zeher, 2016).
Fighting Off Inflammation
Managing inflammation is pivotal in the treatment and management of autoimmune diseases. Strategies include the use of anti-inflammatory drugs, immunosuppressants, and biologics targeting specific immune pathways involved in the inflammatory process. For example, monoclonal antibodies targeting TNF-alpha, a cytokine significantly involved in mediating systemic inflammation, have been effective in treating diseases like rheumatoid arthritis and Crohn's disease. Furthermore, understanding the microbiome's influence on immune responses offers new avenues for therapeutic intervention, as alterations in gut microbiota have been linked to several autoimmune conditions (Wu, Zegarra-Ruiz, & Diehl, 2020).
Section 4 Quiz
1. What initiates the immune system's attack on the body's own cells in autoimmune diseases?
A) External pathogens like bacteria and viruses
B) A breakdown in immunological tolerance due to genetic and environmental factors
C) Direct injury to tissues and organs
D) A surplus production of red blood cells
Click here to reveal the answer.
Correct Answer:: B) A breakdown in immunological tolerance due to genetic and environmental factors.
Explanation:
Autoimmune diseases occur when there's a failure in immunological tolerance, leading the immune system to mistakenly target the body's own cells. This complex interplay between genetic predispositions and environmental triggers results in chronic inflammation and tissue damage.
2. How does inflammation play a role in the development and progression of autoimmune diseases?
A) It signals the body to produce more white blood cells.
B) It acts solely as a protective response to injury.
C) It contributes to tissue damage and exacerbates the disease.
D) It has no significant impact on autoimmune diseases.
Click here to reveal the answer.
Correct Answer:: C) It contributes to tissue damage and exacerbates the disease.
Explanation:
In the context of autoimmune diseases, inflammation is not just a response to tissue injury but a central factor contributing to tissue damage. Chronic inflammation driven by autoimmune activity worsens the condition and can lead to various complications.
3. What role do genetic factors play in the development of autoimmune conditions?
A) They have a minor impact compared to lifestyle choices.
B) Genetic predispositions can significantly influence the risk of developing autoimmune diseases.
C) Only environmental factors are responsible for autoimmune conditions.
D) Genetic factors affect only the severity, not the likelihood, of autoimmune diseases.
Click here to reveal the answer.
Correct Answer:: B) Genetic predispositions can significantly influence the risk of developing autoimmune diseases.
Explanation:
Genetic factors play a crucial role in autoimmune diseases, predisposing individuals to a higher risk of developing these conditions. While environmental triggers are also important, the genetic basis can determine susceptibility to autoimmune responses.
4. Why is managing inflammation important in the treatment of autoimmune diseases?
A) Inflammation has no role in autoimmune diseases and does not need management.
B) Reducing inflammation can alleviate symptoms and prevent further tissue damage.
C) Managing inflammation only helps in improving the physical appearance of symptoms.
D) Inflammation management is only necessary in the initial stages of autoimmune diseases.
Click here to reveal the answer.
Correct Answer:: B) Reducing inflammation can alleviate symptoms and prevent further tissue damage.
Explanation:
In autoimmune diseases, managing inflammation is critical as it helps alleviate symptoms and prevents further damage to tissues caused by chronic inflammatory responses. Effective inflammation management is a key aspect of treatment strategies, improving the quality of life for those affected.
The intricate relationship between inflammation and autoimmunity highlights the importance of understanding immune regulation and the factors that lead to immune system dysregulation. Advances in genetic and molecular biology research continue to unravel the complexities of autoimmune diseases, promising more targeted and effective treatments for managing inflammation and autoimmunity. (Yu et al., 2005), (Chen, Szodoray, & Zeher, 2016), (Wu, Zegarra-Ruiz, & Diehl, 2020).
05. Inflammation's Effect on the Body
Introduction
Chronic inflammation is increasingly recognized as a critical factor in the development of a wide range of diseases. While acute inflammation is a vital part of the body's defense mechanism, chronic inflammation can lead to detrimental effects across various organ systems, contributing to the pathogenesis of numerous age-related and metabolic diseases, as well as cancer.
The Heart
Chronic inflammation plays a pivotal role in the development of cardiovascular diseases. It contributes to the formation of atherosclerotic plaques, which can lead to heart attacks and stroke. Inflammatory cytokines and cells are involved in all stages of atherosclerosis, from the initial endothelial injury to the final rupture of the plaque. The presence of systemic chronic inflammation (SCI) is also a predictor of poor outcomes in patients with cardiovascular disease, highlighting the need for strategies to manage inflammation in order to reduce cardiovascular risk (Furman et al., 2019).
The Brain
Inflammation is also implicated in several neurodegenerative diseases, such as Alzheimer's disease and Parkinson's disease. Chronic inflammation can exacerbate neurodegeneration through the activation of microglia, the resident immune cells of the brain, leading to the release of pro-inflammatory cytokines and neurotoxic substances. This inflammatory process contributes to the progression of neurodegeneration and the clinical manifestations of these diseases.
Metabolic Diseases
Chronic inflammation is a key driver of insulin resistance and type 2 diabetes. Adipose tissue inflammation, in particular, plays a critical role in the development of metabolic syndrome. Inflammatory cytokines interfere with insulin signaling, leading to impaired glucose uptake and increased risk of diabetes. Managing inflammation through lifestyle interventions, such as diet and exercise, can improve insulin sensitivity and help control metabolic diseases.
Cancer
Inflammation contributes to the initiation, progression, and metastasis of cancer. Inflammatory cells and cytokines in the tumor microenvironment promote tumor growth, angiogenesis, and suppression of the immune response against the tumor. Chronic inflammation can also lead to DNA damage, contributing to the mutagenesis that initiates cancer development. Strategies targeting inflammatory pathways are being explored as potential therapies for cancer prevention and treatment.
Section 5 Quiz
1. How does chronic inflammation contribute to the development of cardiovascular diseases?
A) By decreasing cholesterol levels
B) By promoting the formation of atherosclerotic plaques
C) By improving endothelial function
D) By reducing blood pressure
Click here to reveal the answer.
Correct Answer:: B) By promoting the formation of atherosclerotic plaques
Explanation:
Chronic inflammation is a key factor in the development of cardiovascular diseases, primarily through its role in promoting the formation of atherosclerotic plaques. These plaques can lead to heart attacks and stroke by narrowing and hardening the arteries.
2. In what way is inflammation involved in neurodegenerative diseases like Alzheimer's?
A) By protecting neurons from damage
B) By promoting neurogenesis
C) By activating microglia and releasing pro-inflammatory cytokines
D) By improving synaptic function
Click here to reveal the answer.
Correct Answer:: C) By activating microglia and releasing pro-inflammatory cytokines
Explanation:
Inflammation plays a significant role in neurodegenerative diseases such as Alzheimer's by activating microglia, the brain's resident immune cells. This leads to the release of pro-inflammatory cytokines and neurotoxic substances, exacerbating neurodegeneration and contributing to the disease's progression.
3. Describe the role of inflammation in metabolic syndrome and type 2 diabetes.
A) It enhances insulin sensitivity
B) It promotes insulin resistance
C) It increases glucose uptake in tissues
D) It decreases body fat
Click here to reveal the answer.
Correct Answer:: B) It promotes insulin resistance.
Explanation:
Chronic inflammation is a critical driver of insulin resistance, a hallmark of metabolic syndrome and type 2 diabetes. Inflammatory cytokines, particularly from adipose tissue, interfere with insulin signaling, leading to impaired glucose uptake and increased risk of developing these metabolic diseases.
4. Explain the relationship between chronic inflammation and cancer.
A) Inflammation decreases tumor growth and metastasis
B) Inflammatory cells and cytokines in the tumor microenvironment inhibit cancer development
C) Chronic inflammation can lead to DNA damage and promote tumor growth, angiogenesis, and immune suppression
D) Inflammation enhances the immune system's ability to target and destroy cancer cells
Click here to reveal the answer.
Correct Answer:: C) Chronic inflammation can lead to DNA damage and promote tumor growth, angiogenesis, and immune suppression.
Explanation:
Chronic inflammation contributes to cancer initiation, progression, and metastasis. Inflammatory cells and cytokines within the tumor microenvironment support tumor growth and survival, promote the development of new blood vessels (angiogenesis), and suppress the immune response against the tumor, thereby facilitating cancer progression.
Chronic inflammation is a common thread linking a multitude of diseases, highlighting the importance of managing inflammation to improve health outcomes. Understanding the mechanisms by which inflammation contributes to disease can inform the development of targeted therapies to mitigate its harmful effects. (Furman et al., 2019)

